Ulcer causes can include disease or stress, among others. One patient describes what her ulcer felt like—including the red flag she overlooked.
“Here’s How I Knew I Had an Ulcer”: A Patient’s Story, with a Gastro Doctor’s Wisdom
“An ulcer is a breakdown of the interior layer of the stomach or bowel, much like a patch of chipped paint on the wall,” explains Xiaocen Zhang, MD, a gastroenterologist at Tufts Medical Center. “It is fairly common, and can vary in degree of seriousness.” Around 5% to 10% of people will get an ulcer in their lifetime, according to the National Institutes of Health (NIH)—though rates have been steadily declining.
Still, while relatively common, an ulcer gets serious when it is big, deep, damages a blood vessel, or causes the stomach or bowel to deform, Dr. Zhang says. “Occasionally, cancer can present as an ulcer, and without treating or testing for it, you might not know if it is cancer or not.”
This is one reason a patient learned why getting G.I. symptoms checked out is so important.
What an ulcer might feel like, says an expert doctor
It can be difficult to know if you have an ulcer because the signs can vary. Symptoms of an ulcer can mimic other conditions, or you might not experience major changes at all. “Some people feel stomach pain, nausea, gas, or indigestion,” explains Dr. Zhang. Others may get full earlier or lose weight, while some people complain of a sensitive stomach. “Occasionally, an ulcer bleeds and turns people’s stool black or bloody,” she adds.
“These symptoms are common for many different conditions, such as cancer or infection in the abdomen, side effects from medications, or even mental stress,” Dr. Zhang says. Still, “An ulcer can also be silent and cause little discomfort before it gets serious.”
This was the case for one patient, who didn’t know she was dealing with a bleeding ulcer until she went to the hospital for an unrelated issue. Below, she shares the sign she missed—and why she won’t hesitate to seek medical care if it happens again.
How I knew I had an ulcer: A bad case of the flu revealed a different diagnosis
By Linda from Boston, as told by Leslie Finlay, MPA
At 72, Linda was admitted to the hospital for the first time in her life. “I had a very bad case of the flu,” she explains. “It was crazy—I vomited some blood and thought, I’d better go to the hospital.”
“They were doing some tests,” she adds, “and they noticed I was anemic—my [iron] was low. They asked me if I’d had any black stool—and I said yes, as a matter of fact, I was just at the point where I was trying to figure out what was going on with that.”
The symptom I missed
A few months before her hospital visit, Linda had started taking an iron supplement. She loves yoga, but toe cramping made it difficult for her to do certain poses in class. “Of course, they always say, ‘Drink more water’—and I was doing that.” So her yoga teacher suggested upping her iron intake. While iron isn’t necessarily a treatment for muscle cramping, low iron levels can cause weakness, like what Linda was experiencing in her feet, according to the NIH.
Soon, Linda noticed that her stools were starting to look black, and she thought that had something to do with the iron pills she’d started taking. She wasn’t experiencing any other symptoms, so she didn’t think much of it. “But the stool apparently was a big deal.”
She wasn’t entirely wrong to assume a harmless link: Iron supplements are an often benign cause of black poop. In fact, experts say that in some cases, dark stools don’t indicate anything serious—dietary changes and medications like Pepto-Bismol can be other causes.
However, tar-colored stools can also be a sign of serious conditions that require immediate medical attention, including internal bleeding, an abnormal growth like a tumor, or an ulcer.
That’s why Linda now knows that black stools are always a sign to head to the doctor. “My PCP was pretty pissed off at me,” she laughs. “She was like, ‘You’re usually on the ball!’ But I’m a generally healthy person, I’ve never been in the hospital before, I haven’t had any surgeries, I’m active, and I do a lot of yoga and weight-lifting. So, I was kind of dragging my feet, and I wasn’t paying attention. I should have considered it more, just because that’s what you should do with changes happening.”
A surprise ulcer diagnosis
“Other than occasional heartburn, there wasn’t anything really going on with my stomach,” Linda explains. “I know some people who have really bad ulcers, and they have, like, daily pain. And this impacted me very little, I would say.”
So, she was surprised that when seeking treatment for nasty flu symptoms, her doctors grew concerned over a potential ulcer. “Due to the black stool and the low [iron], they scheduled an endoscopy because they said we’ve got to see what’s going on in your digestive system.”
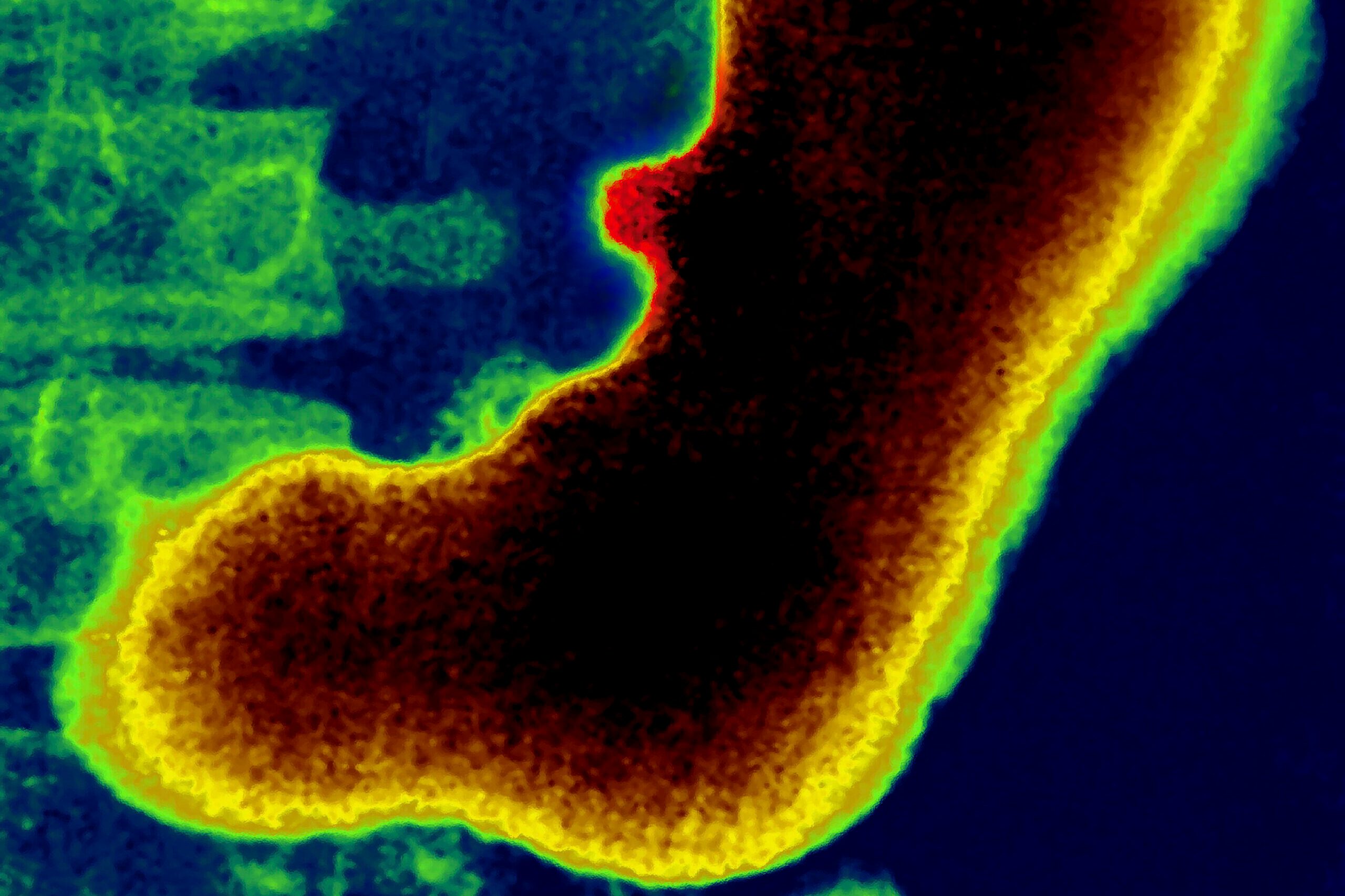
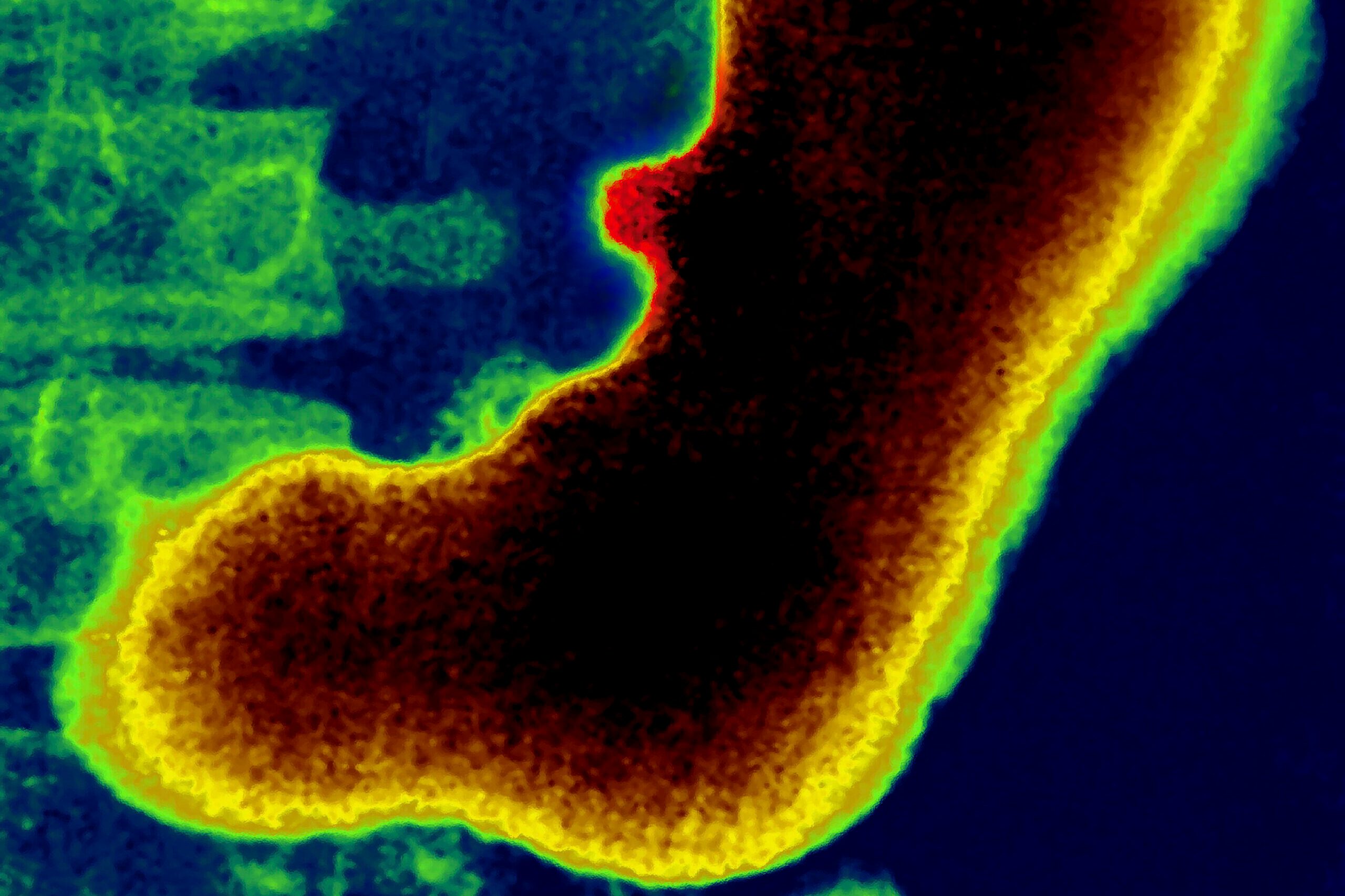
An endoscopy is an exam where a doctor uses a long, thin tube with a tiny camera to get a better look at the gastrointestinal tract. During Linda’s exam, the doctors told her they saw bleeding and diagnosed her with a peptic bleeding ulcer. “I had no idea. I hadn’t had heavy symptoms or anything. But that’s when I discovered I had an ulcer,” she says.
“The doctor prescribed medication that I took twice a day, and that was for three months. And then I had to return for another endoscopy to see how it was going. [My doctor] said it was healing, but it’s not as healed as it should be, so she extended [my treatment]. Now I’m taking one pill a day, and I’m going back for another endoscopy in six months.”
Treatment-wise, Dr. Zhang explains that if an ulcer is caused by an infection, it requires antibiotics. “Other causes of ulcers are usually treated by acid reducer medications,” she says. “It is usually straightforward to treat, unless there is some ongoing issue such as NSAID painkiller use [such as ibuprofen or naproxen] or heavy tobacco or alcohol use.”
What causes ulcers?
Many ulcers are caused by a bacterial infection or overuse of common medications, particularly nonsteroidal anti-inflammatory drugs (NSAIDs). “H.pylori (Helicobacter pylori) is a special type of bacteria that thrives in the acidic stomach environment and is most commonly spread by saliva,” Dr. Zhang explains. “NSAIDs are typically used as painkillers and include ibuprofen, naproxen, and indomethacin.”
She says ulcers can develop from other influences, too:
-
Aspirin can sometimes cause ulcers, especially when used at high doses.
-
Some over-the-counter medications may contain NSAIDs or aspirin, but go by different brand names.
-
Heavy tobacco or alcohol use can cause ulcers.
-
Some people develop ulcers after trauma, a major surgery, or during other periods of physical or mental stress.
Linda says her doctors couldn’t pinpoint one specific cause of her ulcer—as Dr. Zhang explained, a range of factors can contribute to ulcer development. But they did make some recommendations to help her stomach heal and try to prevent problems in the future. “There seemed to be a connection with the iron,” she says. G.I. side effects are common with iron supplements, though an ulcer forming due to taking iron pills is rare, according to 2024 research published in Cureus. Still, to play it safe, Linda lowered the amount she takes.
She’s also stopped taking over-the-counter sleep aids and certain pain medicines, including ibuprofen (Advil), naproxen (Aleve), and Excedrin. For sleep, “[My doctor’s] got me on melatonin in the evening.” When she has pain, she takes acetaminophen (the generic name for Tylenol).
Linda reveals what she thought was a healthy practice may have been irritating the issue: “I also used to drink a lot of lemon and lime in my water,” but she’s stopped doing that to reduce potential irritation to her G.I. system. “And paying attention to stress—stress can always add to [issues].”
What to do if you suspect you have an ulcer
“It is not safe to ‘wait and see’ if you think you might have an ulcer,” Dr. Zhang says. “Ulcers are a lot simpler to deal with when treated early and before a complication arises.”
Linda agrees that the next time something doesn’t look or feel quite right, she won’t wait around. While her ulcer symptoms were subtle, black stool is a red flag you should always get checked out, even if you suspect another explanation. While iron pills can color your stools black, in Linda’s case, they may have been masking a sign of a bleeding ulcer that could have gotten far worse. “Untreated ulcers can create serious problems,” Dr. Zhang explains. “An untreated ulcer can bleed or burrow a hole in the stomach or bowel. It can also cause the digestive tract to deform and create a blockage.”
These complications can be life-threatening, she emphasizes. “Please talk to your doctor if you think you might have an ulcer. There are simple tests, such as stool study or breath analysis, that look for bacterial infection in the stomach. You may need an endoscopy exam to know for sure.”
For daily wellness updates, subscribe to The Healthy by Reader’s Digest newsletter and follow The Healthy on Facebook and Instagram. Keep reading:
About the expert
|




















